15. Carotid Endarterectomy and Stenting
15.1 What is carotid endarterectomy (CEA)
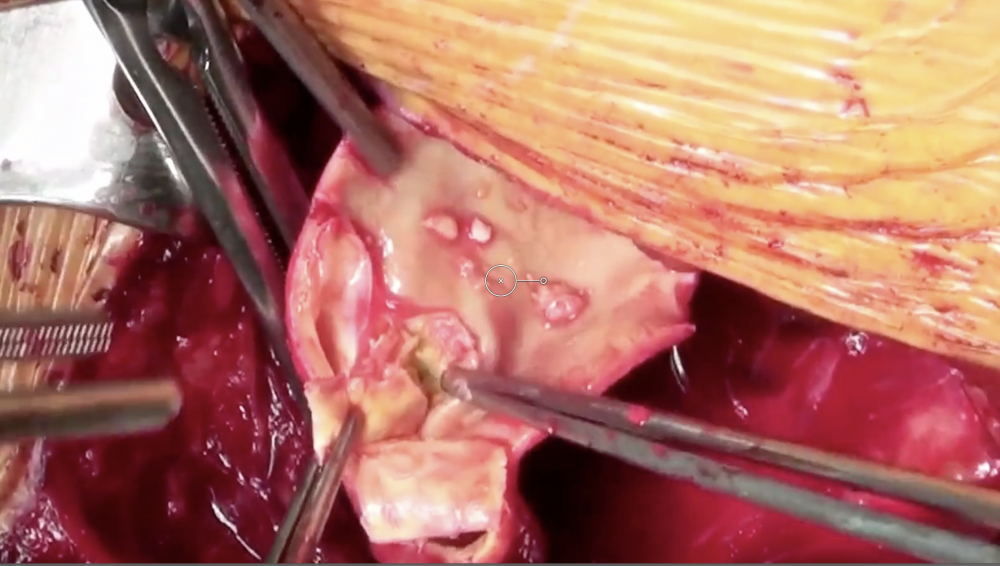
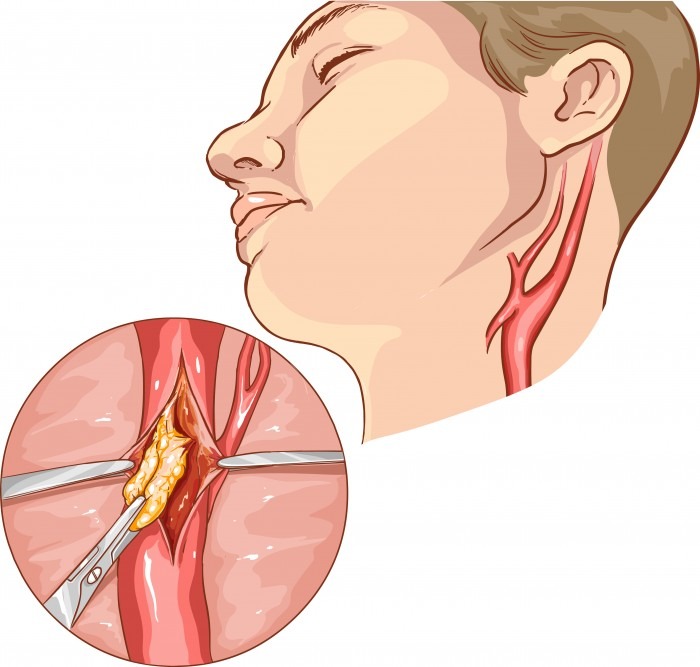
Carotid endaretectomy is a surgical procedure where the carotid artery is opened and the plaque is removed. The procedure allows restoration of blood flow and removal of embolic material to reduce the risk of ischemic / embolic stroke and TIA. There are two main techniques: the classical/conventional method where a patch is used to enlarge the vessel and the eversion method, where the carotid artery is transected at the bifurcation and then everted to remove the plaque. The artery is then repaired by performing an “end-to-end” anastomosis. The procedure is conducted either under local or general anesthesia.
15.2 What are potential complications of carotid endarterectomy
- Stroke (embolic) and death
- Bleeding + haematoma
- Cranial nerve damage (facial nerve, hypoglossal nerve, vagal nerve, superior laryngeal nerve, glossopharyngeal nerve)
- Wound infection
- Hyperperfusion syndrome
- Restenosis
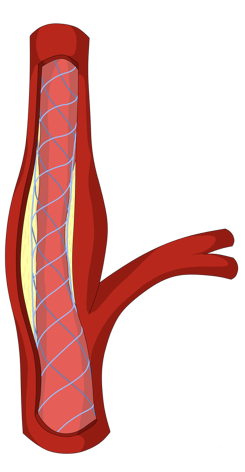
15.3 What is carotid artery stenting?
Carotid stenting is a percutaneous procedure where a stent is placed into the area of stenosis to expand the lumen and prevent vessel recoil. The procedure is performed under fluoroscopic guidance and an embolic protection device. Carotid artery stenting is an alternative to endarterectomy.
15.4 What are potential complications of carotid artery Stenting?
Risks include:
- Stroke and intracranial hemorrrhage and death
- hypoperfuison and bradycardia
- contrast complications
- carotid perforation
- carotid artery dissection.
- Bleeding + haematoma (site of vascular access)
- Acute stent thrombosis (very uncommon)
15.5 When is carotid endarterectomy indicated?
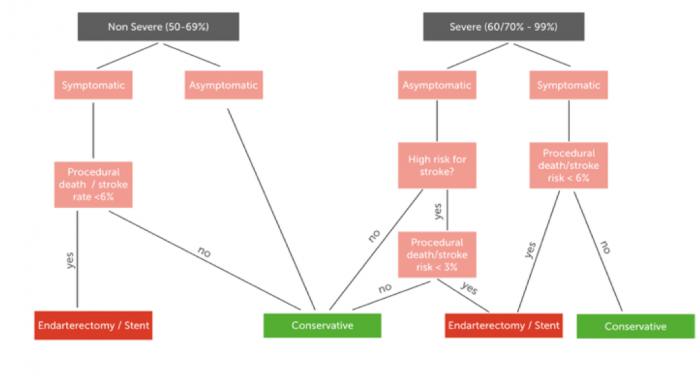
The indication for surgery is always a trade off between the benefit of the procedure and risk. Numerous large randomized studies such as the North American Symptomatic Carotid Endarterectomy Trial Collaborators (NASCET) and the European Carotid Surgery Trial (ECST) have clearly shown the carotid endarterectomy is beneficial in specific patient groups. The following table lists the current indications for this procedure.
- Patients with symptomatic severe (60-99%) stenosis are candidates for endarterectomy (CEA) or stenting if the procedural death / stroke risk is < 6%
- Symptomatic non-severe stenosis (>50%) if the procedural risk is < 6%
- Asymptomatic severe stenosis who are at high risk for stroke if the procedure risk is < 3% (stenosis progression, impaired cerebro- vascular reserve, spontaneous TCD embolisation)
- CEA is contraindicated in patients with < 50% stenosis
- CEA should be performed within 2 weeks of the patient’s last symptoms
- Carotid artery occlusion is NOT an indication for CEA - unless it is an acute occlusion
15.6 Which factors should be considered for carotid endarterectomy and stenting?
There are many other factors which must be considered when deciding if a percutaneous or surgical intervention should be performed.
| Factors to be considered | |
|---|---|
| Neurologic symptoms | TIA? Non-disabling stroke? Stroke? Note that isolated carotid stenosis does not cause vertigo, lightheadedness, or syncope |
| Time since episode | Ideally intervention should be performed within 4 days of an event. CEA is superior if early intervention is possible (within 3-4 weeks). Stenting is superior if late intervention is performed |
| Degree of carotid artery stenosis | 0-99% |
| Location of stenosis | Unilateral - bilateral (higher risk) |
| Stenosis vs occlusion | Collateral flow |
| Co-morbitities | Operative risk, survival? |
| Vascular and local anatomic features | Surgical challenges? |
| Carotid plaque morphology | High-risk plaque? |
If you like the way we teach, please leave a message!