12. Carotid Artery Stenosis Part 2: Spectral Doppler
12.1 How to use Spectral Doppler in the assessment of carotid artery stenosis
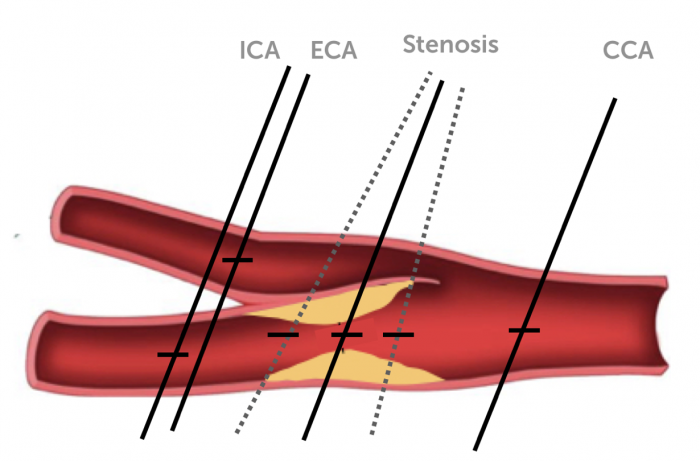
Spectral Doppler should be part of every carotid ultrasound exam. It provides important hemodynamic information and is indispensible for the quantification of stenosis. Measurements should only be performed in a longitudinal view. As a minimal requirement spectral Doppler tracings should be obtained at the following locations:
- Distal common carotid artery (dist. CCA)
- Proximal internal carotid artery (prox. ICA)
- Proximal external carotid artery (prox. ECA)
- Vertebral artery
When using an extended protocol additional measurements can be recorded at:
- Proximal common carotid artery (prox. CCA)
- Mid common carotid artery (mid CCA)
- Mid internal carotid artery (mid ICA)
- Distal internal carotid artery (dist ICA)
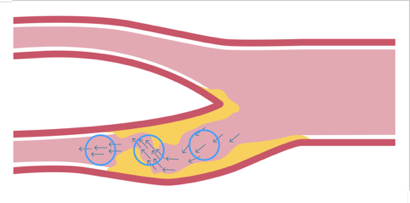
In the presence of a stenosis multiple measurements should be performed at the location of the stenosis in an attempt to record the highest velocities but, also immediately before and after the stenosis. Be aware that the flow direction does not necessarily follow the orientation of the vessel in the presence of a stenosis.
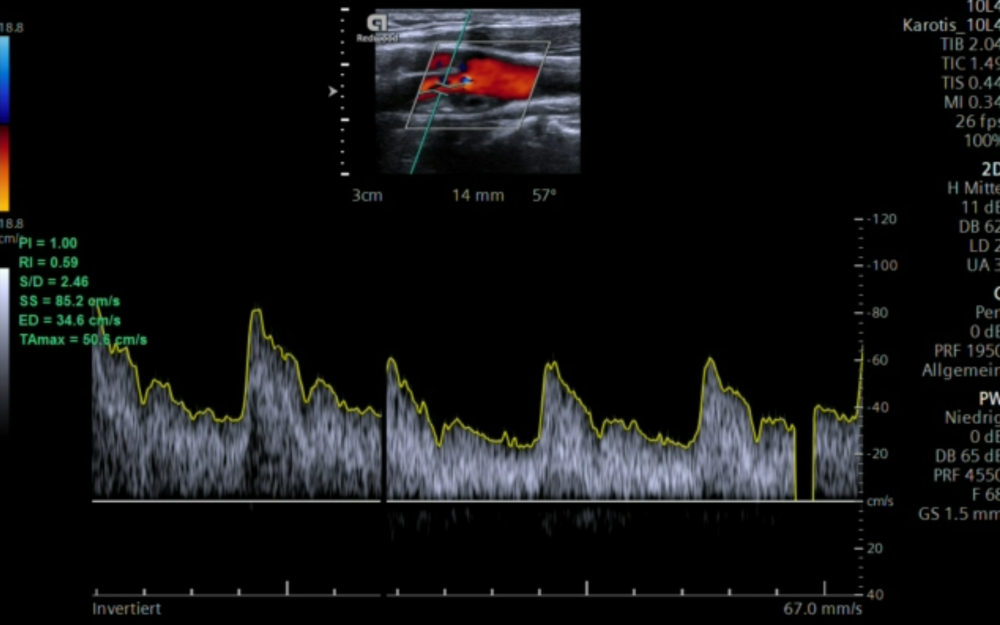
12.2 Which parameters should be obtained from the spectral Doppler Tracing?
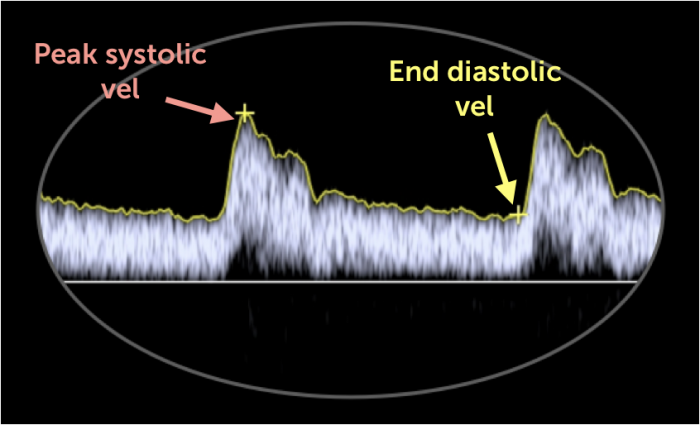
For the quantification of carotid artery stenosis measure both the peak systolic as well as the end diastolic velocity. These velocities will be elevated in the presence of a relevant stenosis. Measurements can be performed manually or with automatic tracing / measurement features.
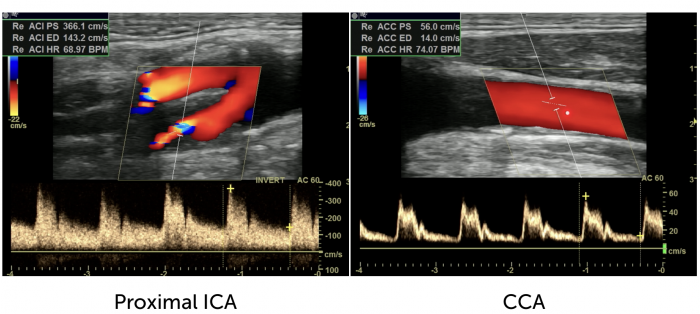
12.3 Which ratios should be calculated
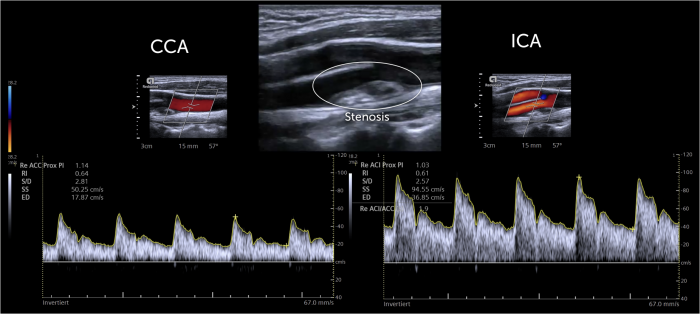
It is important to also calculate velocity ratios. Especially the peak systolic velocity index, which is the ratio between the peak systolic velocity in the ICA vs. the CCA (PSV). In contrast to absolute velocity values of peak systolic and diastolic velocities, ratios are not affected by hypo- or hyperdymamic circulatory states (i.e. hyperdynamic left ventricular function). Ratios are also helpful in the presence of contralateral occlusion. Most scanners provide measurement programs or computer based spectral Doppler tracing algorithms where the ratios are automatically calculated.
Spectral Doppler Ratios
| Parameter | Formula | |
|---|---|---|
| MV | Mean velocity | MV = PSV + 2 EDV / 3 |
| PI | Pulsatility Index (Pourcelot) | PI = PSV - EDV / MV |
| RI | Resistance Index (RI) | RI = PSV - EDV / PSV |
| PSI | Peak systolic Index | PSI = PSVICA/ PSVCCA |
| DI | Diastolic Index | DI = EDVICA / EDVCCA |
| SMR | St. Mary Ratio | SMR = PSVICA / EDVCCA |
Spectral Doppler facts and tips
- Peak systolic velocity is the main parameter used to quantify a stenosis
- Diastolic velocities increase in the internal carotid artery in the presence of a stenosis
- Diastolic velocities decreases in the common carotid artery (CCA) if a stenosis is present in the internal carotid artery because the resistance to flow increases.
- You will see spectral broadening of the signal in stenosis (but also in tortuous vessels)
- Angle correction: the Doppler angle of insonation should be ≤60°
- Measure peak systolic and peak diastolic velocities / calculate ratios
- Don’t use ectopic and post ectopic beats. - Average several beats in atrial fibrillation
- Use automatic measurements only if Doppler quality is good, avoid artefacts
12.4 How can you grade a stenosis of the internal carotid artery based on spectral Doppler?
Doppler based quantification of carotid artery stenosis is widly accepted as the most reliable method. Several grading schemes have been proposed, which vary somewhat with respect to the cutoff values. In general peak systolic velocity that exceeds 125cm/s and a PSV ratio of more than 2 denotes the presence of a stenosis of more than 50%. Very severe severe stenosis (<90) is present if the maximal systolic velocity exceeds 400cm/a and the PSV index is >5.
Note: In near occlusion the flow velocities will drop (trickle flow)
Stenos - grading scheme ICA

With an increase of stenosis we not only see an increase in the systolic velocity but also of diastolic velocities. The following table provides a grading scheme based on diastolic velocities, which can be used in conjunction with the above-mentioned systolic parameters and ratios.
Grading scheme for ICA stenosis based on diastolic velocities
| Stenosis (%) | ICA EDV |
|---|---|
| < 50% | < 40cm/s |
| 50-69 % | > 40 - 100cm/s |
| >70% | >100cm/2 |
12.5 How do you grade common carotid artery stenosis?
Both ratios and peak velocities are also used for the quantification of common carotid artery (CCA) stenosis. One should determine the highest velocity in the stenosis and also measure proximal and distal to the stenosis to calculate the CCA ratio. The following table provides a quantification scheme.
Grading scheme common carotid artery stenosis
| Stenosis (%) | CCA ratio (max systolic vel post/pre stenosis) |
|---|---|
| 0-49% | <2 |
| 50-74 % | ≥ 2 |
| 75-99% | ≥4 |
| occluded | no flow |
12.6 How do you grade external carotid artery stenosis?
Stenosis of the external carotid artery is not uncommon but quantification is usually not as critical since patients are rarely symptomatic and are not at risk of an ischemic event from an external carotid artery stenosis. The external carotid artery however, can provide collaterals in the setting of an ipsilateral carotid artery stenosis or occlusion. The external carotid artery can also be involved in the presence of plaque of the bifurcation, which involves both vessels (ECA and ICA). A stenotic lesion of the external carotid artery should also be described in the report.
The following table provides a grading scheme for external carotid artery (ECA) stenosis.
Grading scheme external carotid artery stenosis
| Stenosis (%) | If ipsilateral < 70% ICA stenosis | If ipsilateral > 70% ICA stenosis |
|---|---|---|
| ≥50% | 130cm/s | ≥ 190cm/s |
| ≥ 75 | 220cm/s | ≥ 200 cm/s |
| occluded | no flow | no flow |
12.7 Which factors influence the velocity in the arteries?
Velocities in the arteries can vary greatly from one individual to another. When assessing flow and quantifying the degree of stenosis it is important to know the potential causes for these variations.
Factors which influence velocites (pitfalls)
| Problem | Cause | Effect |
|---|---|---|
| Vessel size | Large or small vessels, | Lower velocity in larger vessels |
| Vessel geometry | Aneurysms, shape of the bifurcation | Variable effects |
| Age / blood pressure | Hyper and hypotension | Velocity decreases with age, hypertension can increases velocities |
| Contralateral occlusion | Collateral flow | Increased velocities in the contralateral artery |
| Low cardiac output | Heart failure, low flow aortic stenosis, cardiomyopathies | Decrease in velocity |
| High cardiac output | Anxiety, toxic drugs, medication, hyperthyroidism | Increases velocity |
| Beat to beat variations | Atrial fibrillation, ectopic beats | Increase velocities (post ES beat or long RR interval) |
| Aortic regurgitation | Aortic valve dysfunction acute or chronic | Diastolic retrograde flow may influence diastolic parameters (i.e. St. Mary's index) |
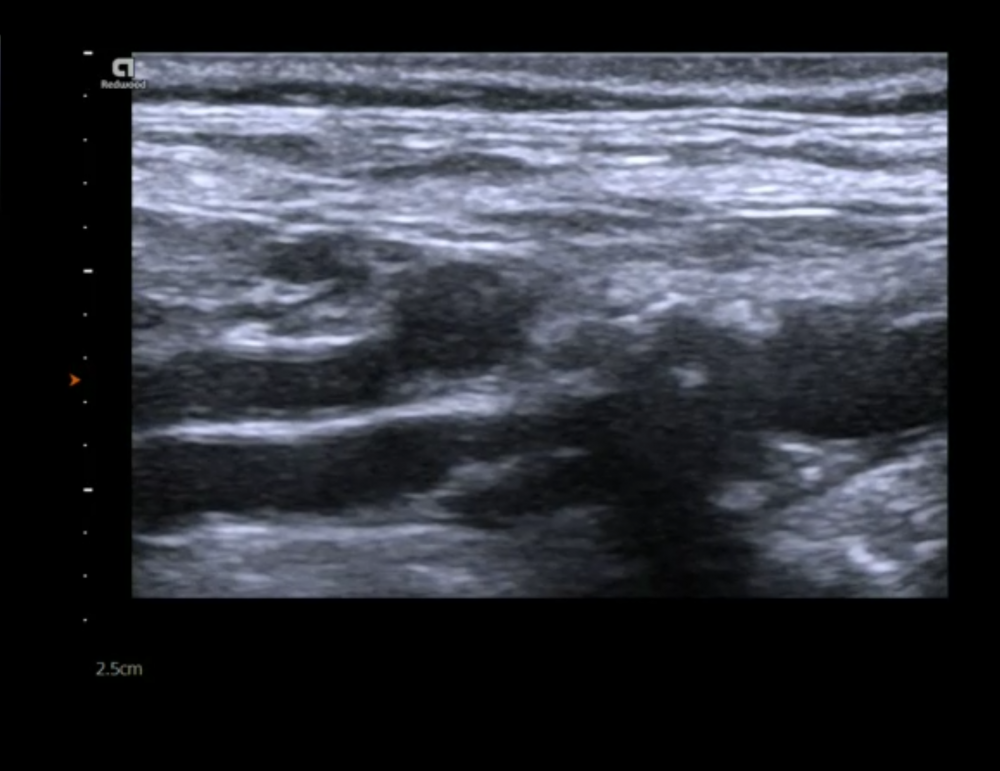
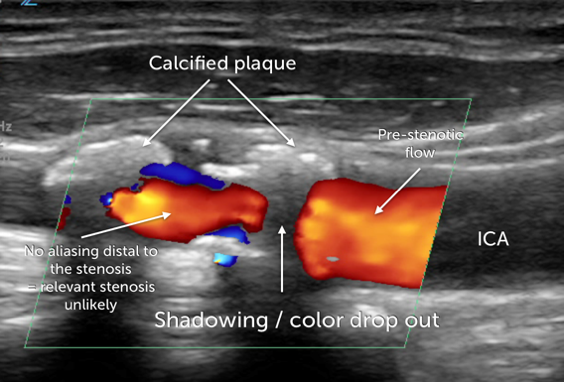
12.8 How do you deal with calcified lesions?
Calcified lesions are more difficult to assess then lesions, which are formed by soft plaque. Acoustic shadowing causes dropouts in both the B mode image and Color Doppler. The quality of the spectral Doppler tracing can also be affected.
- The following table provides some tips on how to assess patients with calcified lesions.
- Use multiple planes to avoid / reduce shadowing
- Use transverse view to check if the calcified plaque is circumferential (this makes it more difficult to quantify stenosis!)
- Look at aliasing / velocity distal to the stenosis. If there is no color flow aliasing or increased velocity then a significant stenosis is unlikely
- A low PSV/EDV ratio distal to the plaque indicates a relevant stenosis
- If a calcified lesion is long (>1cm) then it is not possible to exclude a hemodynamically relevant stenosis - you will need CT or MRI angio
12.9 How can I detect carotid artery occlusion?
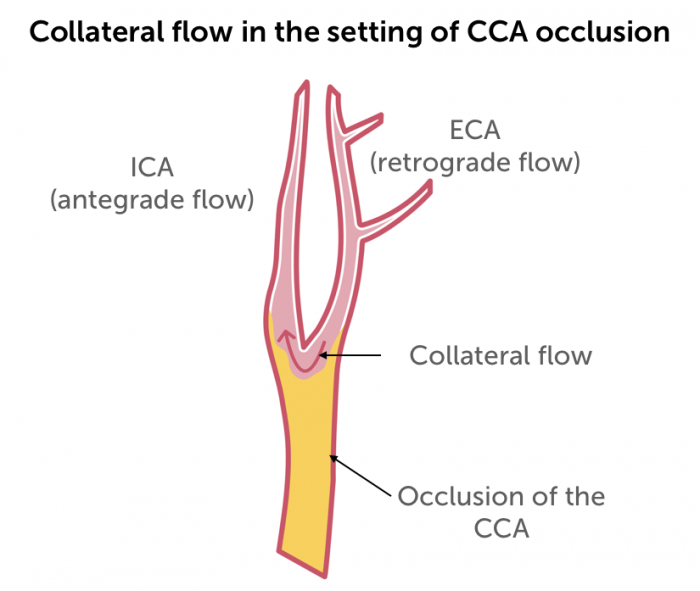
Carotid artery occlusion can be difficult to diagnose. The echogenicity of the occluded lumen is increased and may be difficult to discern from the surrounding tissue. Sometimes you will see a “to-and-fro” motion of the artery. You will only find a weak (trickle flow) or even no Doppler signal (Color and spectral Doppler) The velocities will be low proximal to the occlusion. Flow velocities will be higher in the contralateral CCA. If the ipsilateral CCA is occluded without involvement of the ICA you might be able to see retrograde flow (collateral flow) from the external carotid artery via the bifurcation into the ICA.
If you like the way we teach, please leave a message!