Pediatric Detectives Part 1: Acute Abdominal PAIN

In the atmosphere of the pediatric examination room, the pediatrician turns into a medical detective faced with a single clue that is hard to pinpoint: PAIN. The only testimony to the child's suffering is often the wordless language of pain. So, the examiner must use all his clinical acumen to make the correct diagnosis in order to initiate treatment.
Unlike adults, children, especially the youngest among us, lack the ability to articulate their discomfort and locate pain with precision. The youngest among them only have cries as a means of communication. As they age, they get better at extracting and conveying vital information to make them understand!
Appendicitis is the most frequent reason for acute abdomen in children, and its incidence peaks around 12-14 years of age. At the same time it’s also the most frequently performed abdominal surgery (laparoscopic). Overall, it remains a big global public health challenge (Guan L, Liu Z, Pan G, et al., 1990-2019).
Acute appendicitis is primarily diagnosed clinically, relying on a meticulous patient history and physical examination, especially in pediatric cases. Imaging and lab studies focus on ruling in or ruling out potential diagnoses and confirming suspicions. Ultrasound is the preferred imaging method due to its suitability, but the operator's proficiency is crucial to reach the reported sensitivity of 75-95% and specificity of somewhere around 85-98% (Pedram A, Asadian F, Roshan N., 2019).
This blog series strives to equip you with the tools to accurately detect appendicitis for proper treatment and recognize its mimics to avoid unnecessary invasive procedures!
As a guide for this blog article series (and maybe also your clinical routine), We’d like to introduce you to the mnemonic “PAIN”:
- Patient symptoms, Progression, and Palpation
- Anatomy and Aetiology
- Imaging Appendicitis
- Narrow down your diagnosis!
In this first part of the series, we will review the typical symptoms and clinical features of appendicitis, with a special focus on the physical examination. We’ll also discuss the basic anatomy and sonoanatomy of the appendix and address the aetiology and disease process leading to complications that need surgical intervention. And of course, in the following parts, you will see many ultrasound images with pathological and non-pathological examples that will stick in your mind!
Patient symptoms, Progression, and Palpation
Patient Symptoms – Decipher the Body Language:
- Nausea and Vomiting – often the first symptom in children
- Diffuse abdominal pain – gradually moves into the right lower abdomen
- Relieving posture: Typically, the right leg is bent at the hip and the child refers pain when hopping – the child may limp!
- Sometimes, only uncharacteristic gastroenteritic symptoms like diarrhea...
- Sometimes, only loss of appetite
- Fever
- Leukocytosis and Increased C-reactive protein (CRP)
- The younger the patient is, the less characteristic the symptoms may be!
Progression – Time Course of Symptoms:
- When it comes to acute appendicitis, it is crucial to identify the time of onset of pain. Patients are usually admitted within the first 48 hours of the onset of symptoms. Healthcare professionals must recognize the different stages of acute appendicitis, with the first stage often characterized by inflammation of the inner layer of the appendix and referred to as catarrhal (uncomplicated) appendicitis. At this stage, diagnostic mistakes and unnecessary appendectomies may occur. And, importantly, at this stage, antibiotics can be used as the first treatment option.
- If the symptoms persist for more than 48 hours and sonography shows an appendix with well-differentiated wall layers, the likelihood of complicated appendicitis decreases.
- A sudden pain relief/reduction can be a concerning sign of a possible perforation/rupture. If the appendix perforates, the accumulated pressure is suddenly relieved. The irritating contents spill into the abdominal cavity and lead to peritonitis. This is a complication that requires immediate intervention (AB & Surgery).
Palpation – Hands-on!
-
Localized Tenderness and Rebound Pain:
- Palpation of the lower right abdomen often reveals localized tenderness, and releasing pressure may cause increased pain (rebound tenderness, also called Blumberg sign).
-
Guarding and Rigidity:
- The child may exhibit guarding, a reflex contraction of the abdominal muscles, and rigidity, indicating inflammation of the peritoneum.
-
McBurney's Point Tenderness:
- Tenderness at McBurney's point, located between the belly button and the right hip bone, is a classic sign of appendicitis.
-
Psoas Sign:
- Pain elicited when the child flexes their right hip against resistance may indicate irritation of the psoas muscle, often associated with an inflamed appendix.
-
Rovsing's Sign:
- Pressing on the left lower abdomen and experiencing pain on the right side is a positive Rovsing's sign.
Anatomy and Aetiology
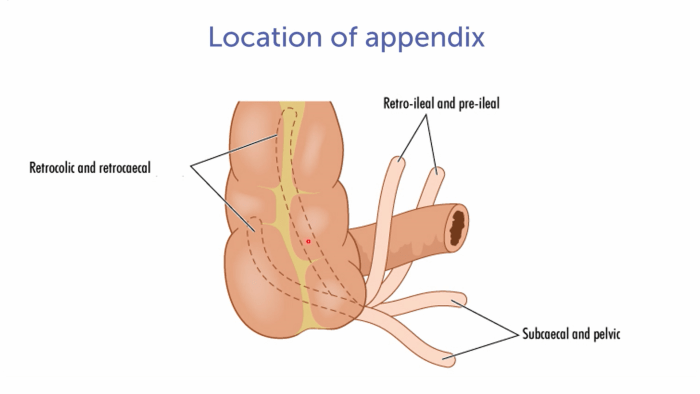
The normal appendix is typically located in the right lower quadrant of the abdomen; more specifically, it originates at the tip of the caecum and then, most frequently, extends some centimeters retrocaecal. However, it can also be found in other locations, such as retrocolic, pelvic or subcaecal, retro-/ or preileal, or even somewhere completely else, like, for example in the left lower quadrant! The location also influences the character and location of pain and other symptoms!
Sonoanatomy or “Help, I can’t find the Appendix!”
The biggest challenge of imaging the appendix is finding it!
- Colon gas is often in your way (patients should fast 6 hours before the exam, with typical pain symptoms they don’t feel like eating anyway). Try to push away the gas with gentle pressure on your ultrasound probe, if the child tolerates it.
- There are quite “funky” locations of the Appendix (as mentioned above)
- Even a normally positioned appendix can be difficult to find if you don’t have enough training!
Normal Sonoanatomy:
Beginning at the hepatic flexure, trace the colon down to the caecum. A more or less typically located appendix can be found on ultrasound near the following sonoanatomical landmarks: The iliac vessels, the terminal ileum, and the cecal pole (more cranially, not seen in the image). Another typical landmark is the psoas muscle found in the far field here! Search for a blind-ending, tubular structure arising from the tip/ the end of the cecum (cecal pole).
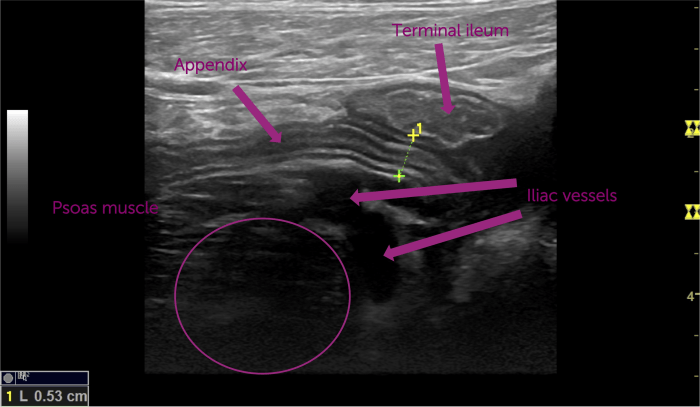

Size:
The normal appendix diameter is typically less than 6 mm. Please note that the range of normal is quite broad, and diameter is not the only thing that matters for diagnosing a pathology! This has also been backed up by CT studies, reporting a range of normal extending to up to 8.7 mm and as much as 39% having an appendix larger than 6 mm in diameter (Trout AT, Towbin AJ, Zhang B., 2014). By the way, the length of a normal appendix, not of great importance for the diagnosis, but interesting to know for your ultrasound exam, ranges from 2-20 cm.
Visualization of Wall Layers:
A healthy appendix typically shows well-differentiated wall layers: The mucosa, submucosa, muscularis propria, and serosa. When viewed in the short axis, a healthy appendix displays different wall layers with distinct echogenicity. The wall thickness is expected to be uniform and generally measures less than 3mm.
Compressibility:
It’s best to check compressibility in a short axis view of the appendix, where a normal appendix looks oval and can be compressed under gentle pressure from the ultrasound probe (Also, it’s quite helpful to see a child's reaction). This contrasts with the surrounding blood vessels, which do not collapse under compression.
Surroundings:
Start scanning at the right upper colon flexure and slide down towards the caecum. Look for normal peristalsis of the intestines indicating regular bowel activity. Assess the surrounding structures for signs of inflammation or fluid collections, which may indicate inflammations.
Color Doppler:
Doppler ultrasound can help assess normal blood flow within the appendix and identify the iliac vessels.
Aetiology of Appendicitis
The exact aetiology of acute appendicitis remains unknown, but the most prevalent hypothesis is some kind of obstruction. The disease process of appendicitis can be described in several stages. Stages 2-5 present clear indications for surgical treatment.
-
Early Stage Appendicitis:
- Obstruction of the appendiceal lumen leads to mucosal edema, ulceration, bacterial growth, appendiceal distention, and increased intraluminal pressure.
- Stimulation of visceral afferent nerve fibers causes mild visceral periumbilical or epigastric pain lasting around 4-6 hours.
-
Suppurative Appendicitis:
- Elevated intraluminal pressures surpass capillary perfusion pressure, causing lymphatic and venous drainage blockage.
- This leads to acute suppurative appendicitis as bacterial and inflammatory fluids invade.
- Contact between the inflamed serosa and the parietal peritoneum triggers a characteristic shift of pain to the right lower abdominal quadrant (RLQ), more intense than the initial visceral pain.
-
Gangrenous Appendicitis:
- Intramural venous and arterial thromboses result in the development of gangrenous appendicitis.
-
Perforated Appendicitis:
- Persistent tissue ischemia leads to appendiceal infarction and eventual perforation.
- A perforated appendix releases infectious material into the abdominal cavity, causing localized or generalized peritonitis.
-
Phlegmonous Appendicitis or Abscess:
- Instead of open perforation, an abscess may form body's attempt to contain the infection.
- An inflamed or perforated appendix can be limited by the adjacent greater omentum or the loops of the small intestine.
-
Spontaneously Resolving Appendicitis:
- Relief from the obstruction of the appendiceal lumen may result in the spontaneous resolution of appendicitis (spontaneous expulsion of an appendicolith from the lumen). Uncomplicated acute appendicitis can resolve under antibiotic treatment. Note that at times, the initial (sonographic) presentation may mimic appendicitis and is later often identified as so-called lymphoid hyperplasia.
- Pedram A, Asadian F, Roshan N. Diagnostic Accuracy of Abdominal Ultrasonography in Pediatric Acute Appendicitis. Bull Emerg Trauma. 2019;7(3):278-283. doi:10.29252/beat-0703011
- Trout AT, Towbin AJ, Zhang B. Journal club: The pediatric appendix: defining normal. AJR Am J Roentgenol. 2014;202(5):936-945. doi:10.2214/AJR.13.11030
Stay tuned! In the next part, we’ll discuss in more detail how these stages translate into ultrasound imaging results!
A special thanks to our 123Ambassador Andrei Satsuk, MD, for providing a pediatric sonoanatomy image of an appendix from his clinical practice! Instagram: @satsuk_md

