How to image patients with congenital heart disease - Part 1
Do you know what you should look for on the echocardiography in patients with the referral “congenital defect”? Often these patients look fine and don’t know which defect they have. They only know that a “heart defect” was diagnosed in infancy or childhood.
The truth is that most individuals will end up having no defect. The diagnostic tools which were available 40 or 50 years ago were far from perfect, and it seems the diagnosis of a congenital defect was made far too often in the past.
But, be aware that patients with congenital defects can remain asymptomatic until late in life. In such patients, you might be the one who is the first to make the diagnosis.
Which congenital defects are common in the adult population, and how can you diagnose them?
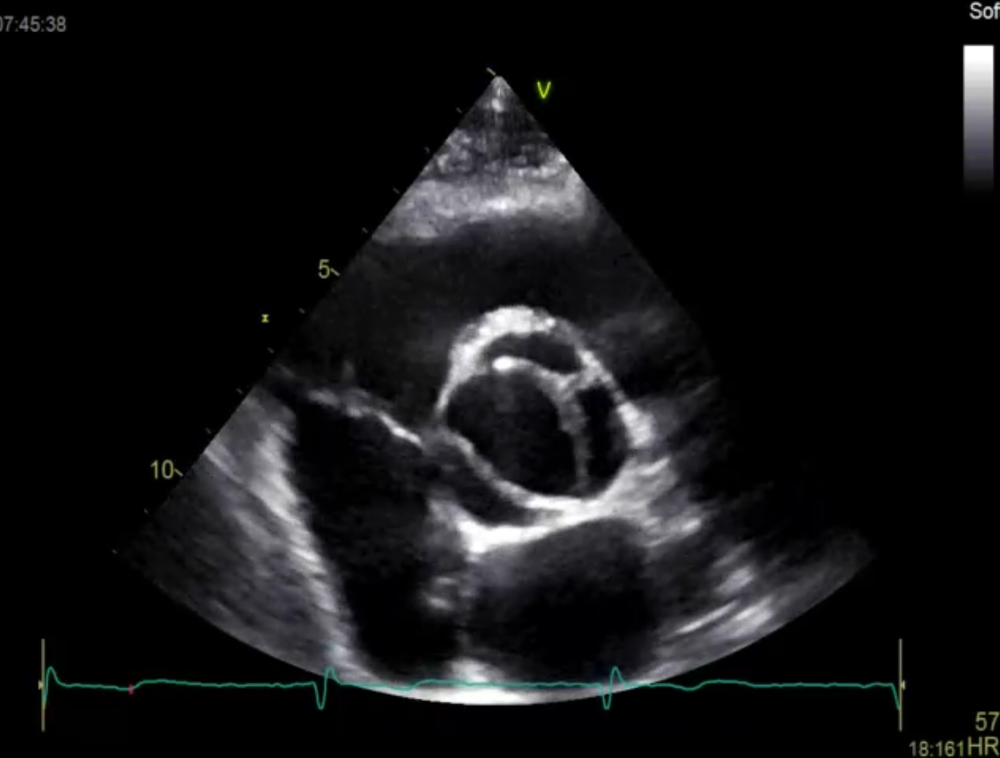
How to image congenital abnormalities of the aortic valve
The most common congenital abnormalities in the adult population are aortic valve pathologies such as bicuspid aortic valves. It affects 1,3% of the population. Consequently, the likelihood of finding such an abnormality is relatively high!
+ Imaging Tips:
Specifically look at the opening motion of the aortic valve; use the high frame rate images, and scroll back and forward. Functional bicuspid valves (valves with a raphe) may appear tricuspid on a still image. Look for a higher than normal AV velocity. Be aware that mild forms of aortic stenosis are not uncommon. Look for eccentric aortic regurgitation jets (AR is frequently present in congenitally abnormal valves.
How to image atrial septal defects
The prevalence of atrial septal defect is 1 to 2 per 1000 live births. If the defect is significant or associated with other abnormalities, it is usually detected early in life. But not always. In adults, you might also see relevant ASD II defects or sinus venous defects. And you can find small secundum defects, which can go unnoticed and not require treatment.
+ Imaging Tips:
Always perform atypical views where the interatrial septum is perpendicular to the ultrasound beam. For this reason, you should also try a subcostal view. These views will allow you to visualize the ASD jet. But even atypical orientations will not help you detect an upper sinus venosus defect. For this reason, it is essential to look at the size of the right ventricle. In right ventricular dilatation, you must always exclude an ASD! The next step is then a contrast study and Qp:Qs calculations!
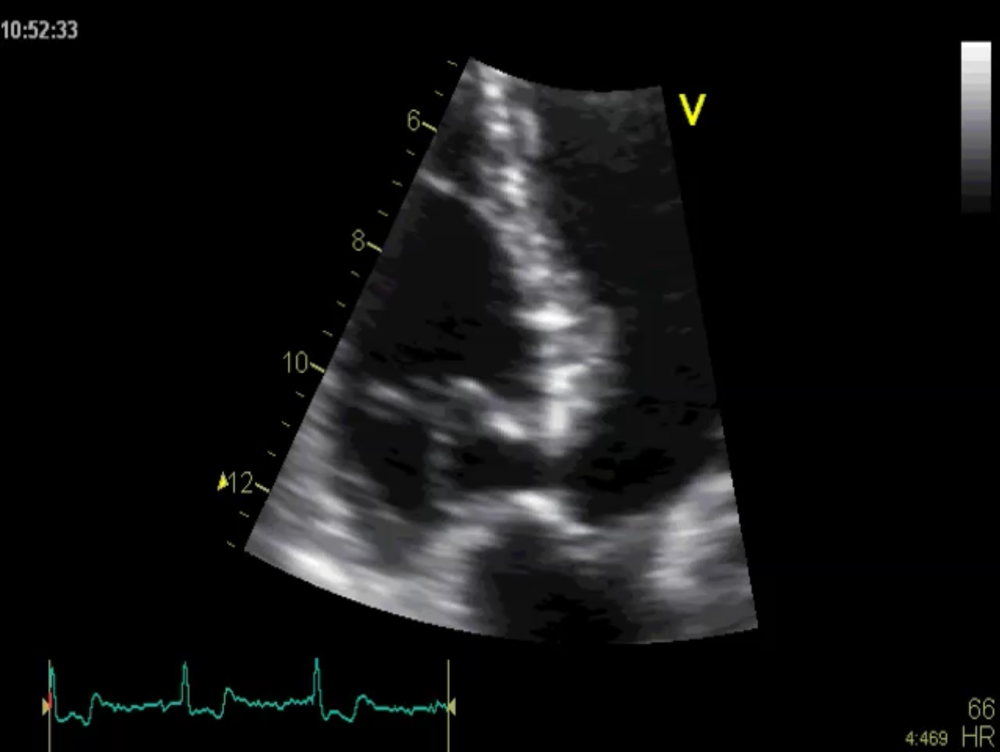
How to image ventricular septal defects
Ventricular septal defects occur in approximately 0.1-0.4 of all live births. Most Large defects will be diagnosed during fetal echocardiography or early in life. In particular, if pulmonary hypertension or Eisenmenger is present and if the VSD is part of another congenital abnormality (i.e., Fallot Tetrology, atrioventricular septal defects, transposition of the great arteries). As a result, you will most commonly find small restrictive defects in an adult population, either in the membranous or muscular septum.
+ Imaging Tips:
A membranous VSD is best seen in a short axis at the base of the heart, just slightly below the aortic valve. The short axis view is also the best imaging plane in most patients to measure the peak VSD velocity with CW Doppler. Also, use a 5- chamber view to display the membranous septum. Note that a VSD can close spontaneously during life. In these patients, you might see tricuspid valve tissue, which fully (or partially) covers the defect. The sealed defect has an aneurysmatic appearance.
For this reason, we call this pathology: an aneurysmal transformation of the IVS. Below is such an example. Small Muscular defects are often challenging to find. But it helps if you use atypical views and image planes that avoid foreshortening. Remember, muscular defects can sometimes be very distal in the interventricular septum.
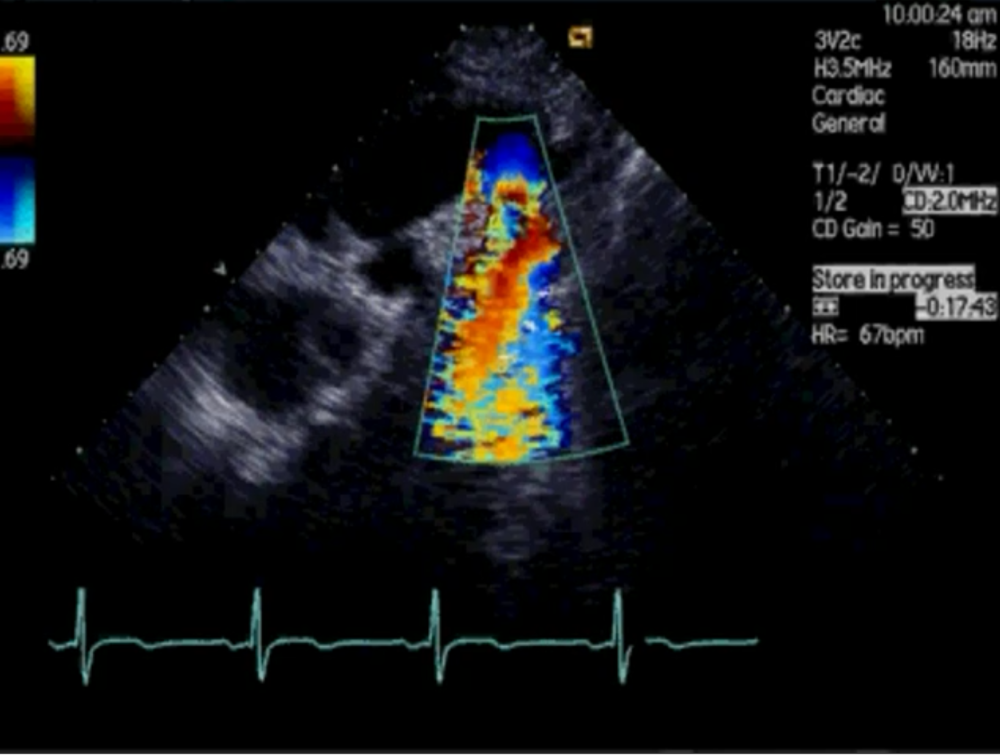
How to image Coarctation
Coarctation is the least common defect that we have discussed so far. It occurs in 1 of 2500 births. Adult patients with coarctation typically present with systemic hypertension. Be alert if young patients present with left ventricular hypertrophy and hypertension. Here it is mandatory to rule out coarctation as a treatable cause of hypertension.
+ Imaging tip:
Look for coarctation in the region of the ductus arteriosus distal to the left subclavian artery. Image this region from a suprasternal window. Then, align the transducer to the aortic arch and use the color Doppler to locate the coarctation site. Color Doppler also allows you to guide continuous wave Doppler. Also, if you find coarctation, look for a bicuspid aortic valve, which is commonly associated with this pathology.
If you want even more than sign up for our full Adult Congenital Heart Disease BachelorClass.
Stay tuned for part 2 of this series.
Thomas Binder and the 123sonography team