11. Carotid Artery Stenosis Part 1: B mode and Color flow
11.1 Introduction
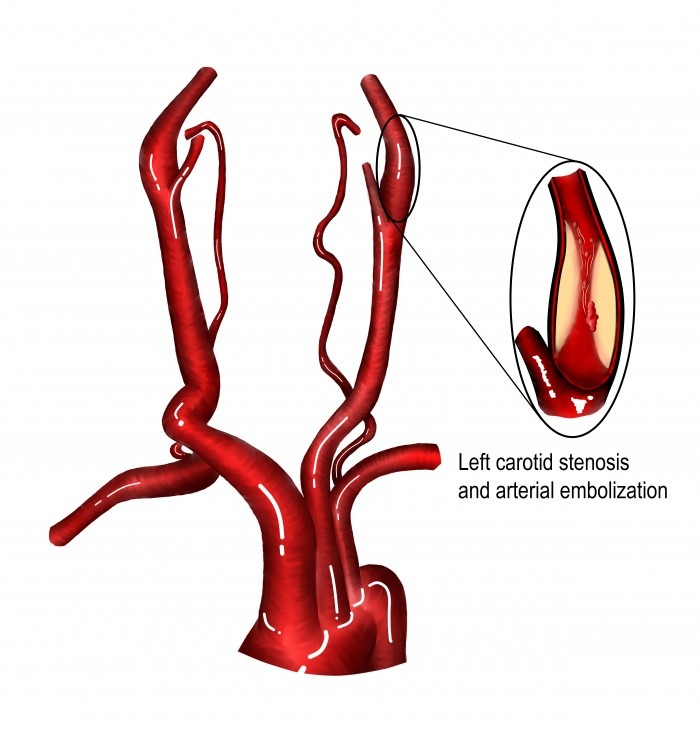
Carotid artery stenosis is defined as a narrowing of the carotid artery, in most cases as the result of atherosclerosis and plaque formation. Carotid artery stenosis (>50%) is present in approximately 5% of the elderly population (>75 years). The transition from a plaque to a stenosis occurs gradually and there is no consensus on when we still speak of a plaque and when “stenosis” begins. Probably when the degree of narrowing is more than 30-50%. The presence of a stenosis does not necessarily mean that blood flow to the brain is impaired. Impairment of flow usually begins if the degree of stenosis exceeds 60- 70%.
For the management of patients (surgery, stenting, medication) it is important to differentiate between symptomatic and asymptomatic stenosis (based on the presence or absence of neurologic symptoms).
11.2 What is the clinical relevance of carotid artery stenosis?
Carotid artery stenosis plays an important role as a cause of stroke. The risk of ipsilateral stroke at 5 years is 8% if the degree of stenosis is < 60% and 16.2% if stenosis is 60-99%. The presence of plaque and stenosis is also a marker of general atherosclerosis. Patients with carotid artery disease are more likely to have significant coronary artery disease. The prevalence of carotid artery stenosis in patients with coronary artery disease been reported to be as high as 25.4% (depending on which population is studied). The risk of a major cardiovascular event (death or myocardial infarction) is increased threefold even in patients who are asymptomatic.
Therefore, the detection of a stenosis has large implications and should prompt a thorough work up to also search for the presence of coronary artery disease and peripheral artery disease.
11.3 What is the role of ultrasound in carotid artery stenosis?
Ultrasound is the primary diagnostic tool to screen for carotid artery disease. It is simple, inexpensive and widely available. Especially the area of the bifurcation, where the wide majority of stenotic lesions are located can easily be assessed with ultrasound. Compared to other imaging modalities such as CT-Angiography, Digital subtraction Angiography and Magnetic resonance Angiography Carotid ultrasound also allows hemodynamic assessment of stenosis. In most situations ultrasound can be used as the sole method for the assessment and follow up of carotid artery stenosis.
11.4 When should other imaging modalities be used?
The following table lists the advantages and disadvantages of the various imaging modalities (Ultrasound, CT Angiography, MRI Angiography and Digital subtraction Angiography)
Comparison imaging modalities for the assessment of carotid artery stenosis
| Modality | Application | Advantage | Disadvantage |
|---|---|---|---|
| Ultrasound | Screening technique, plaque morphology, quantification of stenosis (haemodynamics), follow up | Inexpensive, safe, availability vessel wall can be seen (wall morphology, IMT), provides haemodynamic information | Operator dependant, cranial vessels can not be visualized |
| CT - Angiography | Confirmation of stenosis, quantification not possible with ultrasound i.e. (calcified lesions), planning of interventional- and surgical procedures. Visualization of intracranial vessels | Fast image acquisition, Also allows assessment of non vascular structures, unlimited viewing angles, vertebral arteries can always be visualized, displays aortic arch and intracranial segments. Operator independent. | Side effects of contrast (i.e. kidney, allergy), radiation. Automatic quantification techniques, quantification of stenosis only based on morphology, extensive calcifications can be a problem |
| MRI Angiography | Confirmation of stenosis, quantification not possible with ultrasound (i.e. calcified lesions), planning of interventional and surgical procedures. Visualization of intracranial vessels, especially when brain ischemia should also be assessed. | Also allows assessment of non vascular structures, ideal to simultaneously assess stroke and ischemia. Vertebral arteries can always be visualized, no radiation, calcifications are not a problem, contrast less toxic than that of CT | Expensive, availability, contraindication to some implants, more sensitive to artifacts, side affects to contrast. Claustrophobia |
| Digital subtraction Angiography | During interventional procedures | Visualization of the entire carotid artery system, high resolution, small vessels can be displayed | Invasive (risk of stroke), side effects of contrast, radiation (higher than CT angiography) |
In clinical practice additional imaging modalities are indicated if:
- Image quality is poor and one is not certain if a stenosis is present or not
- Ultrasound does not allow a reliable quantification of the degree of stenosis (especially in severely calcified lesions)
- A intracranial stenosis / occlusion is suspected
- To assess collaterals
- Symptomatic carotid artery disease for preoperative/interventional planning
- CT Angiography in combination with intracranial CT to correlate intracranial vascular disease with the findings of CT Angiography/Ultrasound and to correlated them with symptoms
- In acute stroke (is thrombolysis feasible?)
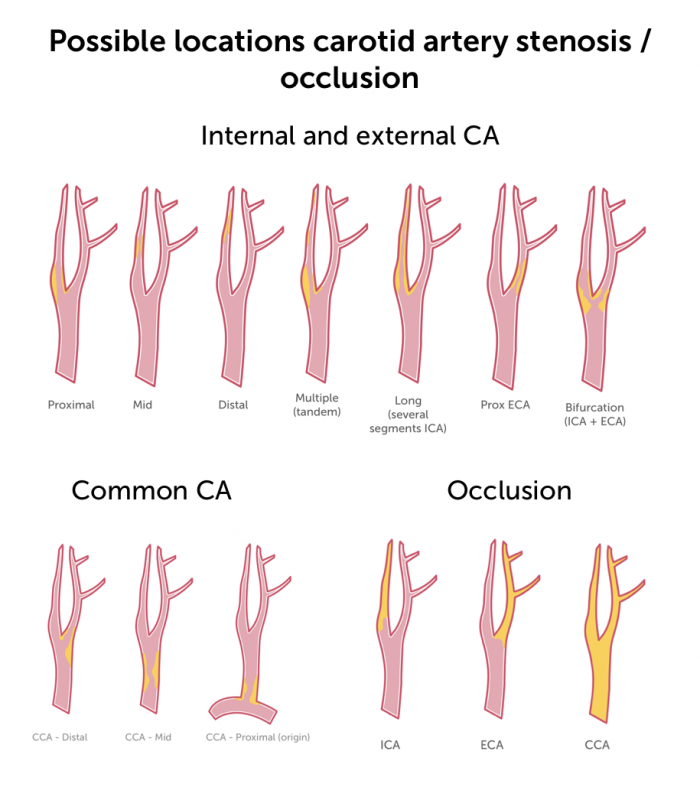
11.5 Where is a carotid artery stenosis most commonly located?
A stenosis can be present in any part of the vessel, but by far the most common site is the area of the bulb (bifurcation) and the proximal carotid artery. The proximal common carotid artery is the second most common site of stenosis. It causes approximately 1-2% of all cerebral ischemic strokes.
Location of stenosis
- Most common in the proximal ICA (bulb)
- Distal internal carotid artery uncommon (consider fibromuscular dysplasia)
- Mid internal carotid artery segment can be involved in long or tandem stenosis
- Plaque build up in the bifurcation can lead to proximal ICA and ECA stenosis
- Patients with ECA stenosis are not at risk of stroke
- Beware stenotic lesions can be hidden within tortuous vessels
11.6 How to quantify the degree of stenosis – “eyeballing”
It is important to first get a rough estimate of the degree of the stenosis (eyeballing)
Step 1: You first need to detect and locate the region with a lumen reduction. It is important to do this in both a transverse and a longitudinal view. Since an eccentric stenosis can be missed if only a longitudinal view is applied.
Step 2: Optimize your image quality and turn up the gain so you don’t miss soft plaque
Step 3: Tilt the transducer back and forth in the longitudinal view
Step 4: Slide the transducer up and down in a transverse view to spot the area with the greatest lumen reduction
Step 5: get a rough estimate on how much the lumen reduction is present
Step 6: Use Color Doppler to search for flow turbulences. Higher flow velocities and the jet will not only help you to detect the site of stenosis but it also points to a stenosis which is more than 50%.
Step 7: Use other Doppler modalities or B Mode flow to better assess the stenosis. The flow information often allows you to better depict the lumen. This can be done both in a longitudinal and a transverse view.
Note: NEVER use eyeballing alone, but with experience it will allow you to match your impression to other methods of quantification (hemodynamic).
11.7 How to quantify carotid artery stenosis with B-Mode:
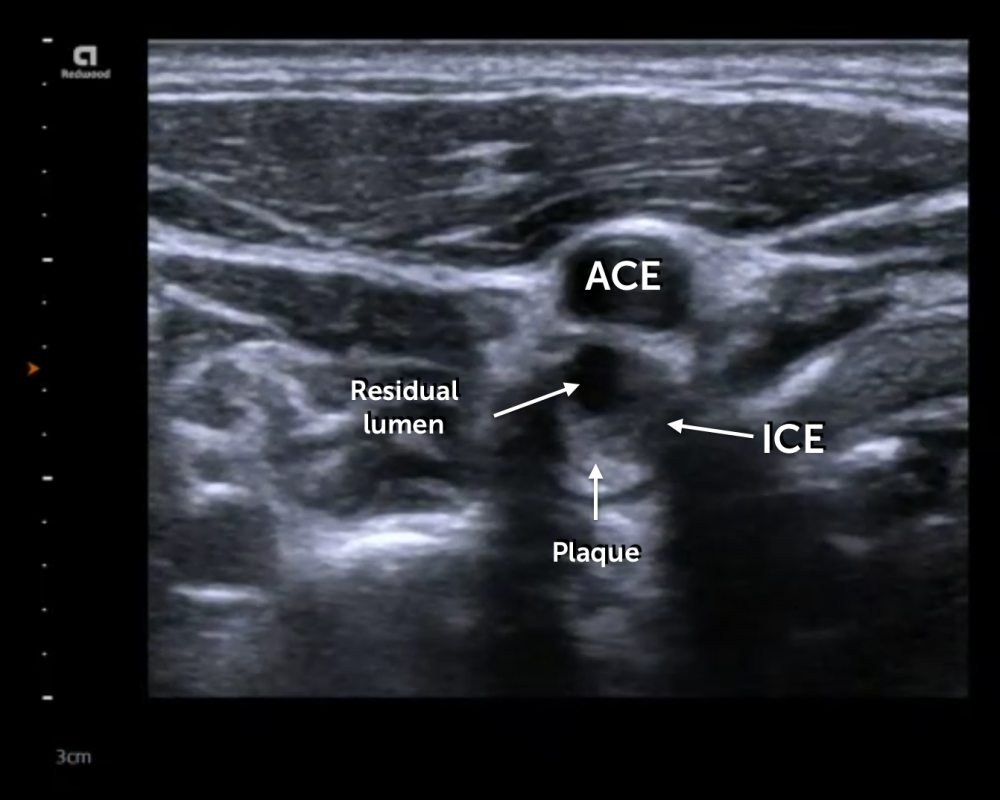
The degree of stenosis can be calculated both in a transverse and a longitudinal view. To quantify the stenotic lesion in a transverse view one can use both the area and the diameter method. In principle one measures the area (or diameter) of the entire vessel as well as the area (or diameter) of the residual lumen. The percent (%) of area (or diameter) reduction is then calculated from these measurements. A “70% stenosis “ would then mean that the lumen of the artery is reduced by 70%.
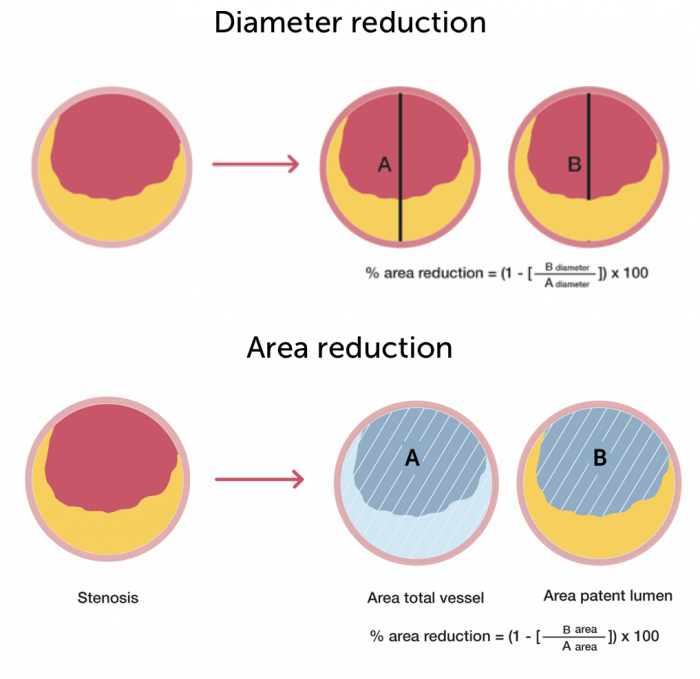
Pitfalls and problems of transverse
- Often difficult to trace / measure the diameters and areas
- Sometimes difficult to determine where the area with the smallest lumen is
- Calculations based on diameter measurements are inaccurate in eccentric plaque
- Calcified plaques can not be assessed (shadow)
- NOTE: This methodology is rarely used in ultrasound. Mostly performed in radiology and research
11.8 How to quantify carotid artery stenosis with the NASCET/ECST methods
The NASCET and ECST quantification method are based on criteria, which were used in large clinical trials to quantify stenotic lesions. They are based on diameter measurements. These methods are mostly used in research and are applied in CT/MRI Angiography, less commonly in ultrasound. Note: As all B Mode measurements, they to not provide any hemodynamic information.
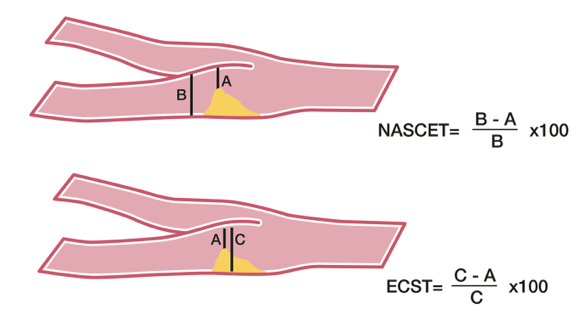
NASCET / ECST Facts:
- NASCET = North American Symptomatic Carotid Endarterectomy Trial - studied the outcome after endarterectomy
- ECST = European Carotid Surgery Trial - compared surgery with a conservative approach in symptomatic patients
- Measurements are calculated from longitudinal views
- The ECST formula compares the total diameter of the artery at the site of stenosis with the residual lumen diameter3
- The NASCET formula compares the diameter of the artery distal to the site of stenosis with the residual lumen diameter
- ECST usually yields higher values for the degree of stenosis
- NASCET correlates better to hemodynamic and angiography, ECST reflects better the plaque burden
- Tip: most scanners have the formulas integrated into their measurement programs.
- Problems: time consuming, does not account for eccentricity of stenosis, calcified plaque difficult to quantify
- Conversion formula ECST to NASCET: ECST (%) = 0.6x NASCET(%) + 40%
11.9 How to use Color Doppler in the assessment of carotid artery stenosis
11.8 How to use Color Doppler in the assessment of carotid artery stenosis
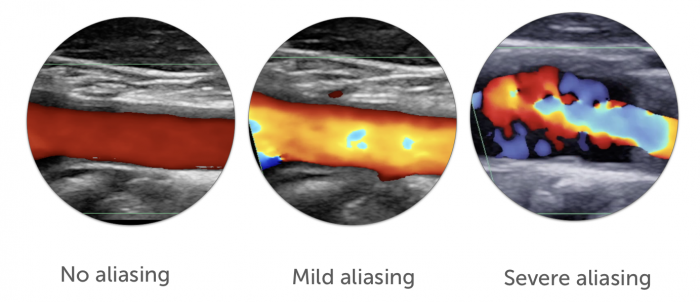
Color Doppler (as well as Power Doppler) helps to delineate the lumen (i.e. to detect a sparing defect). This is especially useful in the presence of soft plaque (which are hypoechoic) and can easily be missed. Color Doppler is also used to guide the placement of the spectral Doppler sample volume.
Note: You will have color Doppler dropouts in the presence of calcified lesions (ultrasound shadowing)
If you like the way we teach, please leave a message!